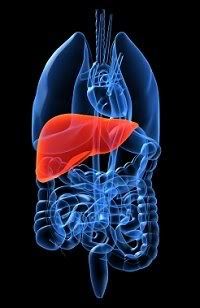
 The use of herbal products has become one of the biggest trends in recent years, as more “natural” drug therapy becomes popular. There are over 29,000 products available on the market. One reason for this is the rise in costs of perscription medication . The public believes that herbal supplements are harmless and reliable for treating or preventing many diseases. A major concern about herbal supplements is the risk of side effects. The FDA does not regulate their use, and the research on them is slim to none. The drugs are placed on the market on a trial and error basis, without any review of the benefits or risks. The producers of herbal supplements are not required to post warnings on labels; this has led to severe liver hepatotoxicity and damage to other organ systems.
The use of herbal products has become one of the biggest trends in recent years, as more “natural” drug therapy becomes popular. There are over 29,000 products available on the market. One reason for this is the rise in costs of perscription medication . The public believes that herbal supplements are harmless and reliable for treating or preventing many diseases. A major concern about herbal supplements is the risk of side effects. The FDA does not regulate their use, and the research on them is slim to none. The drugs are placed on the market on a trial and error basis, without any review of the benefits or risks. The producers of herbal supplements are not required to post warnings on labels; this has led to severe liver hepatotoxicity and damage to other organ systems.Health professionals and the makers of herbal supplements are at odds on this subject. Because of the public view about herbal medication and the "all natural ingredients", use of these supplements has doubled over the last ten years. Between 20% to 30% of consumers have been admitted to a hepatic-clinic for liver injury. Ironically enough, herbal medications seem to be used most by people who have liver diseases.
The risk to the liver can be severe. Cases that have been reported liver injury from mild, emergency transplant, and even death. This can be a surprising fact to most of the public, considering that the consensus of herbal supplements is harmless. In a public survey, 1 out of every 6 consumers report taking an herbal supplement in conjunction with their current prescriptions. This can be a dangerous combination!
There are thousands of stories about this herbal supplement side effects. The major concerns seem to be hepatotoxicity, especially associated with herbal products taken before surgery and use of these medications by the elderly. There are so many herbal products that it is almost impossible to list them along with potential side effects here; however, the number one injury most often cited is to the liver. Hepatotoxicity is at greater risk when acetaminophin and herabal supplements are taking together. Some of the most dangerous herbal drugs to the liver are; Black cohosh, Kava, Echinacea.
The lesson of the day: ask your healthcare provider before combining any drugs, perscriptioin or over-the-counter, with herbal medications.
Are you at risk??
References:
Barger, L. Herbs and Pain Relievers Don't Mix: The Dangers of Mixing Herbal Supplements and OTC Pain Relivers. Retrieved October 22, 2009. http.//herbalmedicine.suite101.com
Larson, A. Hepatotoxicity Due to Herbal Medications. Retrieved October 22, 2009. www.uptodate.com/patients



Set plates on the bottom shelf to one side in another cabinet. Next to the plates, add the saucers. Place all soup bowls on the top shelf above the plates and saucers.Food Display Cabinets
ReplyDeleteIf you take herbal supplements and are about to undergo surgery you should stop taking them prior to surgery and discuss which supplements you have been taking with your doctor. Male Enhancement
ReplyDelete